Hip Arthroscopy
Arthroscopy is a surgical procedure that gives doctors a clear view of the inside of a joint. This helps them diagnose and treat joint problems.
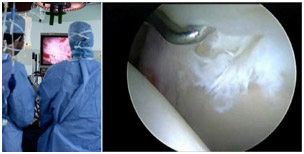
During hip arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your hip joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments.
Hip arthroscopy has been performed for many years, but is not as common as knee or shoulder arthroscopy.
During arthroscopy, your surgeon can see the structures of your hip in great detail.
(Right) Small instruments are used to clean up a labral tear.
Anatomy
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thigh bone).
A slippery tissue called articular cartilage covers the surface of the ball and the socket. It creates a smooth, frictionless surface that helps the bones glide easily across each other.
The acetabulum is ringed by strong fibrocartilage called the labrum. The labrum forms a gasket around the socket.
The joint is surrounded by bands of tissue called ligaments. They form a capsule that holds the joint together. The undersurface of the capsule is lined by a thin membrane called the synovium. It produces synovial fluid that lubricates the hip joint.
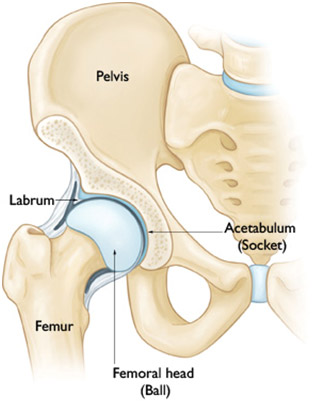
In a healthy hip, the femoral head fits perfectly into the acetabulum.
When Hip Arthroscopy is Recommended
Your doctor may recommend hip arthroscopy if you have a painful condition that does not respond to nonsurgical treatment. Nonsurgical treatment includes rest, physiotherapy and medications or injections that can reduce inflammation. Inflammation is one of your body’s normal reactions to injury or disease. In an injured or diseased hip joint, inflammation causes swelling, pain, and stiffness.
Hip arthroscopy may relieve painful symptoms of many problems that damage the labrum, articular cartilage, or other soft tissues surrounding the joint. Although this damage can result from an injury, other orthopaedic conditions can lead to these problems, such as:
- Femoroacetabular impingement (FAI) is a disorder where bone spurs (bone overgrowth) around the socket or the femoral head cause damage.
- Dysplasia is a condition where the socket is abnormally shallow and makes the labrum more susceptible to tearing.
- Snapping hip syndromes cause a tendon to rub across the outside of the joint. This type of snapping or popping is often harmless and does not need treatment. In some cases, however, the tendon is damaged from the repeated rubbing.
- Synovitis causes the tissues that surround the joint to become inflamed.
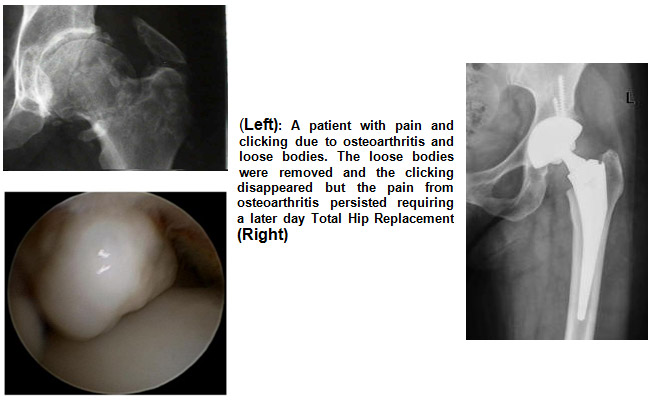
- Loose bodies are fragments of bone or cartilage that become loose and move around within the joint.
- Hip joint infection
Planning for Surgery
If you are having arthroscopy, you will need a physical examination from a physician to assess your health. He or she will identify any problems that may interfere with the surgery.
If you have certain health risks, a more extensive evaluation may be necessary before your surgery. Be sure to inform your orthopaedic surgeon of any medications or supplements that you take. He or she may tell you which medications to stop and which to take prior to surgery.
Most patients spend one night in hospital after a hip arthroscopy although you may go home the same day. This depends on a number of factors.
The hospital or surgery center will contact you ahead of time to provide specific details of your procedure. Make sure to follow the instructions on when to arrive and especially on when to stop eating or drinking prior to your procedure.
Prior to your surgery, you will be evaluated by your anaesthetist. The most common types of anaesthesia are general anaesthesia (you are put to sleep) or spinal, epidural, or regional nerve block anaesthesia (you are awake but your body is numb from the waist down). The anaesthetist, with your input, will determine which type of anaesthesia will be best for you.
Surgical Procedure
At the start of the procedure, your leg will be put in traction. This means that your hip will be pulled away from the socket enough for your surgeon to insert instruments, see the entire joint, and perform the treatments needed.
After traction is applied, your surgeon will make a small puncture in your hip (about the size of a buttonhole) for the arthroscope. Through the arthroscope, he or she can view the inside of your hip and identify damage.

(Left) Your surgeon inserts the arthroscope through a small incision about the size of a buttonhole.
(Right) Other instruments are inserted to treat the problem.
Your surgeon will insert other instruments through separate incisions to treat the problem. A range of procedures can be done, depending on your needs. For example, your surgeon can:
- Clean up and smoothen a labral tear
- Remove loose fragments of bone and cartilage
- Smooth off torn cartilage or repair it
- Trim bone spurs caused by FAI
- Remove inflamed synovial tissue
The length of the procedure will depend on what your surgeon finds and the amount of work to be done.
Complications
Complications from hip arthroscopy are uncommon. Any surgery in the hip joint carries a small risk of injury to the surrounding nerves or vessels, or the joint itself. The traction needed for the procedure can stretch nerves and cause numbness, but this is usually temporary.
There are also small risks of infection, as well as blood clots forming in the legs (deep vein thrombosis).
Recovery
After surgery, you will stay in the recovery room for 1 to 2 hours before being taken back to your hospital bed or discharged home. You will need someone to drive you home and stay with you at least the first night. You can also expect to be on crutches, or a walker, for some period of time.
Rehabilitation
Your surgeon will develop a rehabilitation plan based on the surgical procedures you required. In some cases, crutches are necessary, but only until any limping has stopped. If you required a more extensive procedure, however, you may need crutches for 1 to 2 months.
In most cases, physiotherapy is necessary to achieve the best recovery. Specific exercises to restore your strength and mobility are important. Your physiotherapist can also guide you with additional do’s and dont’s during your rehabilitation.

Long-Term Outcomes
Many people return to full, unrestricted activities after arthroscopy. Your recovery will depend on the type of damage that was present in your hip.
For some people, lifestyle changes are necessary to protect the joint. An example might be changing from high impact exercise (such as running) to lower impact activities (such as swimming or cycling). These are decisions you will make with the guidance of your surgeon.
Sometimes, the damage can be severe enough that it cannot be completely reversed and the procedure may not be successful.
(Left): A patient with pain and clicking due to osteoarthritis and loose bodies. The loose bodies were removed and the clicking disappeared but the pain from osteoarthritis persisted requiring a later day Total Hip Replacement (Right)
Future Developments
Arthroscopy has helped physicians and researchers better understand many hip joint problems. As surgical techniques evolve, it is anticipated that hip arthroscopy will play a greater role in diagnosing and treating hip disease.