Total Knee Replacement
If your knee is severely damaged by arthritis or injury, it may be hard for you to perform simple activities, such as walking or climbing stairs. You may even begin to feel pain while you are sitting or lying down.
If nonsurgical treatments like medications and using walking supports are no longer helpful, you may want to consider total knee replacement surgery. Joint replacement surgery is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume normal activities.
Knee replacement surgery was first performed in 1968. Since then, improvements in surgical materials and techniques have greatly increased its effectiveness. Total knee replacements are one of the most successful procedures in all of medicine.
Whether you have just begun exploring treatment options or have already decided to have total knee replacement surgery, this article will help you understand more about this valuable procedure.
Anatomy
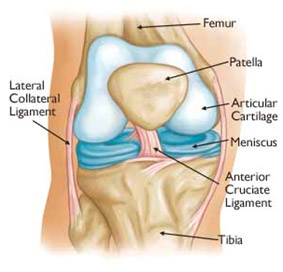
Normal knee anatomy
The knee is the largest joint in the body and having healthy knees is required to perform most everyday activities.
The knee is made up of the lower end of the thighbone (femur), the upper end of the shinbone (tibia), and the kneecap (patella). The ends of these three bones where they touch are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily.
The menisci are located between the femur and tibia. These C-shaped wedges act as “shock absorbers” that cushion the joint.
Large ligaments hold the femur and tibia together and provide stability. The long thigh muscles give the knee strength.
All remaining surfaces of the knee are covered by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage, reducing friction to nearly zero in a healthy knee.
Normally, all of these components work in harmony. But disease or injury can disrupt this harmony, resulting in pain, muscle weakness, and reduced function.
Common Causes of Knee Pain
The most common cause of chronic knee pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis are the most common forms.
- Osteoarthritis. This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older, but may occur in younger people, too. The cartilage that cushions the bones of the knee softens and wears away. The bones then rub against one another, causing knee pain and stiffness.
- Rheumatoid arthritis. This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed “inflammatory arthritis.”
- Post-traumatic arthritis. This can follow a serious knee injury. Fractures of the bones surrounding the knee or tears of the knee ligaments and Meniscus may damage the articular cartilage over time, causing knee pain and limiting knee function.
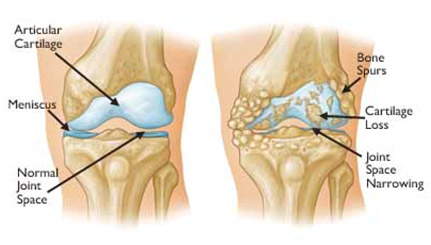
Osteoarthritis often results in bone rubbing on bone with bone spur formation
Description
A knee replacement (also called knee arthroplasty) might be more accurately termed a knee “resurfacing” because only the surface of the bones are actually replaced.
There are four basic steps to a knee replacement procedure.
- Prepare the bone. The damaged cartilage surfaces at the ends of the femur and tibia are removed along with a small amount of underlying bone.
- Position the metal implants. The removed cartilage and bone is replaced with metal components that recreate the surface of the joint. These metal parts may be cemented or “press-fit” into the bone.
- Resurface the patella. The under-surface of the patella (kneecap) is cut and resurfaced with a plastic button. Sometimes the Patella is not resurfaced and this depends on each patient’s specific requirements.
- Insert a spacer. A medical-grade plastic spacer is inserted between the metal components to create a smooth gliding surface.
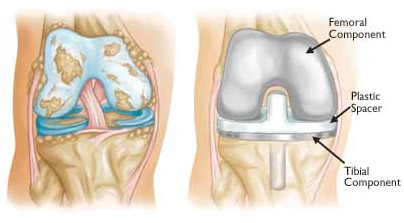
(Left) Severe osteoarthritis
(Right) The arthritic cartilage and underlying bone has been removed and resurfaced with metal implants on the femur and tibia. A plastic spacer has been placed in between the implants. The patellar component is not shown for clarity
Is Total Knee Replacement for You?
The decision to have total knee replacement surgery should be a cooperative one between you, your family, your local doctor and your orthopaedic surgeon. Your local doctor may refer you to an orthopaedic surgeon for a thorough evaluation to determine if you might benefit from this surgery.
Candidates for Surgery
There are no absolute age or weight restrictions for total knee replacement surgery.
Recommendations for surgery are based on a patient’s pain and disability, not age. Most patients who undergo total knee replacement are age 40 to 80, but orthopaedic surgeons evaluate patients individually. Total knee replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
When Surgery Is Recommended
There are several reasons why your doctor may recommend knee replacement surgery. People who benefit from total knee replacement often have:
- Severe knee pain or stiffness that limits your everyday activities, including walking, climbing stairs, and getting in and out of chairs. You may find it hard to walk more than a few blocks without significant pain and you may need to use a cane or walker
- Moderate or severe knee pain while resting, either day or night
- Chronic knee inflammation and swelling that does not improve with rest or medications
- Knee deformity — a bowing in or out of your knee
- Failure to substantially improve with other treatments such as anti-inflammatory medications, cortisone injections, lubricating injections, physiotherapy, or other surgeries

A knee that has become bowed as a result of severe arthritis
The Orthopaedic Evaluation
An evaluation with an orthopaedic surgeon consists of several components:
- A medical history. Your orthopaedic surgeon will gather information about your general health and ask you about the extent of your knee pain and your ability to function.
- A physical examination. This will assess knee motion, stability, strength, and overall leg alignment.
- X-rays. These images help to determine the extent of damage and deformity in your knee.
- Other tests. Occasionally blood tests, or advanced imaging such as CT Scans and magnetic resonance imaging (MRI) scan, may be needed to determine the condition of the bone and soft tissues of your knee.

(Left) In this x-ray of a normal knee, the space between the bones indicates healthy cartilage (arrow)
(Right) This x-ray of an arthritic knee shows severe loss of joint space and bone spurs (arrows)
Deciding to Have Knee Replacement Surgery
Talk With Your Doctor
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether total knee replacement is the best method to relieve your pain and improve your function. Other treatment options — including medications, injections, physiotherapy or other types of surgery — will also be considered and discussed.
In addition, your orthopaedic surgeon and his team will explain the potential risks and complications of total knee replacement, including those related to the surgery itself and those that can occur over time after your surgery.
Never hesitate to ask your doctor and his team questions when you do not understand. The more you know, the better you will be able to manage the changes that knee replacement surgery will make in your life.
Realistic Expectations
An important factor in deciding whether to have total knee replacement surgery is the understanding what the procedure can and cannot deliver. Most people who undergo total knee replacement surgery experience a dramatic reduction of knee pain and a significant improvement in the ability to perform common activities of daily living. But total knee replacement will not allow you to do more than you could before you developed arthritis.
With normal use and activity, every knee replacement implant begins to wear in its plastic spacer. Excessive activity or weight may speed up this normal wear and may cause the knee replacement to loosen and become painful. Therefore, most surgeons advise against high-impact activities such as running, jogging, jumping, contact sport or other high-impact activities.
Realistic activities following total knee replacement include unlimited walking, swimming, golf, driving, hiking, cycling, dancing and other low-impact sports.
With appropriate activity modification, knee replacements can last for many years.
Preparing for Surgery
Medical Evaluation
If you decide to have total knee replacement surgery, your orthopaedic surgeon may ask you to have a medical evaluation by a cardiologist or another specialist before your surgical procedure. This is needed to make sure you are healthy and fit enough to have the surgery and complete the recovery process. This is likely to be required for older patients and those with chronic medical conditions, such as heart disease.
Tests
Several tests, such as blood and urine samples, an electrocardiogram (ECG), and chest x-rays, may be needed to help plan your surgery.
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact your orthopaedic surgeon for treatment to improve your skin before surgery
Medications
Tell your orthopaedic surgeon and his team about the medications you are taking. He or your local doctor will advise you which medications you should stop taking and which you can continue to take before surgery.
Weight Loss
If you are overweight, your doctor may ask you to lose some weight before surgery to minimise the stress on your new knee and possibly decrease the risks associated with your knee replacement surgery.
Dental Evaluation
Although infections after knee replacement are not common, an infection can occur if bacteria enter your bloodstream. Because bacteria can enter the bloodstream during dental procedures, major dental procedures (such as tooth extractions and periodontal work) should be completed before your knee replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Urinary Evaluations
People with a history of recent or frequent urinary infections should have a urological evaluation before surgery. Older men with prostate disease should consider completing required treatment before undertaking knee replacement surgery.
Social Planning
Although you will be able to walk on crutches or a walker soon after surgery, you will need help for several weeks with such tasks as cooking, shopping, bathing and laundry.
If you live alone, your orthopaedic surgeon’s team, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended care facility (Rehabilitation hospital) during your recovery after surgery may also be arranged.
Home Planning
Several modifications can make your home easier to navigate during your recovery. The following items may help with daily activities:
- Safety bars or a secure handrail in your shower or bath
- Secure handrails along your stairways
- A stable chair for your early recovery with a firm seat cushion (and a height of 45 to 50 cm), a firm back, two arms, and a footstool for intermittent leg elevation
- A toilet seat riser with arms, if you have a low toilet
- A stable shower bench or chair for bathing
- Removal of all loose carpets and cords from the areas where you walk in your home
- A temporary living space on the same floor because walking up or down stairs will be more difficult during your early recovery
Set up a “recovery centre” where you will spend most of your time. Things like the phone, television remote control, reading materials and medications should all be within reach.

Your Surgery
You will be admitted to hospital either the night before, or on the day of your surgery.
Anaesthesia
Prior to your surgery, you will be evaluated by your anaesthetist. The most common types of anaesthesia are general anaesthesia (you are put to sleep) or spinal, epidural, or regional nerve block anaesthesia (you are awake but your body is numb from the waist down). The anaesthetist, with your input, will determine which type of anaesthesia will be best for you.
Implant Components
Many different types of designs and materials are currently used in artificial knee joints. All of them consist of 4 basic components: the Femoral component attached to the lower end of the Femur, the Tibial component attached to the top end of the Tibia, a medical grade plastic spacer placed between these 2 components and sometimes a medical grade plastic component placed on the back of the Patella.
The prosthetic components may be “press fit” into the bone to allow your bone to grow onto the components or they may be cemented into place. The decision to press fit or to cement the components is based on a number of factors, such as the quality and strength of your bone. A combination of cemented and non-cemented components may also be used.
Your orthopaedic surgeon will choose the type of prosthesis that best meets your needs.

Different types of knee implants are used to meet each patient’s individual needs
Procedure
The procedure itself takes a few hours. Your orthopaedic surgeon will remove the damaged cartilage and bone, and then position the new metal and plastic implants to restore the alignment and function of your knee.
After surgery, you will be moved to the recovery room where you will remain for several hours while your recovery from anaesthesia is monitored. After you wake up, you will be taken to your hospital room.
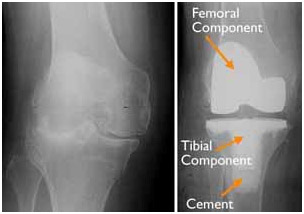
(Left) An x-ray of a severely arthritic knee
(Right) The x-ray appearance of a total knee replacement. Note that the plastic spacer between the bones does not show up in an x-ray
Your Stay in the Hospital
You will most likely stay in the hospital for several days.
Pain Management
After surgery, you will feel some pain, but your anaesthetist and nurses will provide medication to make you feel as comfortable as possible. Pain management is an important part of your recovery. Movement will begin soon after surgery, and when you feel less pain, you can start moving sooner and get your strength back more quickly. Talk with your Orthopaedic and anaesthetic teams if postoperative pain becomes a problem.
Physiotherapy
Walking and light activity are important to your recovery and will begin the day of or the day after your surgery. Most patients who undergo total knee replacement begin standing and walking with the help of a walking support and a physiotherapist the day after surgery. The physiotherapist will teach you specific exercises to strengthen your knee and entire leg and restore movement for walking and other normal daily activities. He or she will also instruct you on very important precautions to avoid complications.

A Physiotherapist educating a patient on the use of a walking frame
Preventing Pneumonia
It is common for patients to have shallow breathing in the early postoperative period. This is usually due to the effects of anaesthesia, pain medications, and increased time spent in bed. This shallow breathing can lead to a partial collapse of the lungs (termed “atelectasis”) which can make patients susceptible to pneumonia. To help prevent this, it is important to take frequent deep breaths. Your may be provided with a simple breathing apparatus called a spirometer to encourage you to take deep breaths.

Spirometer
Recovery
The success of your surgery will depend largely on how well you follow your medical team’s instructions during your hospital stay and more importantly during the first six weeks after surgery when you have been discharged from the acute care hospital.
Wound Care
You may have stitches or staples running along your wound or a dissolvable suture beneath your skin. The stitches or staples will be removed approximately 2-3 weeks after surgery.
Avoid getting the wound wet until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.

Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron and Vitamin C supplements, is important to promote proper tissue healing and restore muscle strength. Be sure to drink plenty of fluids.

Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal activities of daily living within 3 to 6 weeks following surgery. Some pain with activity and at night is common for several weeks after surgery.

Your activity program should include:
- A graduated walking program to slowly increase your mobility, initially in your home and later outside
- Resuming other normal household activities, such as sitting, standing, and climbing stairs
- Specific exercises several times a day to restore movement and strengthen your knee. You may be able to perform the exercises without help, but the majority of patients require the help of a physiotherapist at a physiotherapy centre especially during the first few weeks after surgery
You will most likely be able to resume driving when your knee bends enough that you can enter and sit comfortably in your car, and when your muscle control provides adequate reaction time for braking and acceleration. Most people resume driving approximately 6 weeks after surgery.
Possible Complications of Surgery
The complication rate following total knee replacement is low. Serious complications, such as a knee joint infection, occur in fewer than 2% of patients. Major medical complications such as heart attack or stroke occur even less frequently. Chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur, they can prolong or limit full recovery.
Discuss your concerns thoroughly with your orthopaedic surgeon prior to surgery.
Infection
Infection may occur superficially in the wound or deep around the prosthesis. It may happen while in the hospital or after you go home. It may even occur years later.
Minor infections of the wound are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis. Any infection in your body can spread to your joint replacement.
Blood Clots
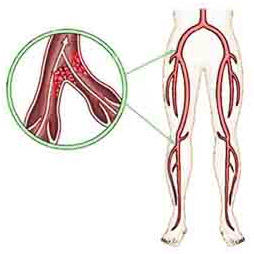
Blood clots may develop in leg veins
Blood clots in the leg veins are the most common complication of knee replacement surgery. These clots can be life-threatening if they break free and travel to your lungs. Foot and ankle movement is encouraged immediately following surgery to increase blood flow in your leg muscles to help prevent leg swelling and blood clots.
Your orthopaedic surgeon will outline a prevention program which may include blood thinning medications, support compression stockings, inflatable leg coverings, ankle pump exercises, and early mobilisation.

Implant Problems
Although implant designs and materials, as well as surgical techniques, continue to advance, implant surfaces may wear down and the components may loosen. Additionally, although an average of 115° of motion is generally anticipated after surgery, scarring of the knee can occasionally occur, and motion may be more limited, particularly in patients with limited motion before surgery.
Continued Pain
A small number of patients continue to have pain after a knee replacement. This complication is rare, however, and the vast majority of patients experience excellent pain relief following knee replacement.
Neuro-Vascular Injury
While rare, injury to the nerves or blood vessels around the knee can occur during surgery.
Avoiding Problems after Surgery
Blood Clot Prevention
Follow your orthopaedic surgeon’s instructions carefully to reduce the risk of blood clots developing during the first several weeks of your recovery. He or she may recommend that you continue taking the blood thinning medication you started in the hospital. Notify your doctor immediately if you develop any of the following warning signs.
Warning signs of blood clots. The warning signs of possible blood clots in your leg include:
- Increasing pain in your calf
- Tenderness or redness above or below your knee
- Increasing swelling in your calf, ankle, and foot
Warning signs of pulmonary embolism. The warning signs that a blood clot has traveled to your lung include:
- Sudden shortness of breath
- Sudden onset of chest pain
- Localized chest pain with coughing
Preventing Infection
A common cause of infection following total knee replacement surgery is from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your knee replacement and cause an infection.
After your knee replacement, you must take preventive antibiotics before dental or surgical procedures that could allow bacteria to enter your bloodstream.
Warning signs of infection. Notify your doctor immediately if you develop any of the following signs of a possible knee replacement infection:
- Persistent fever (higher than 38 Degrees Celsius Orally)
- Shaking chills
- Increasing redness, tenderness, or swelling of the knee wound
- Drainage from the knee wound
- Increasing knee pain with both activity and rest
Avoiding Falls
A fall during the first few weeks after surgery can damage your new knee and may result in a need for further surgery. Stairs are a particular hazard until your knee is strong and mobile. You should use a cane, crutches, a walker, hand rails, or have someone to help you until you have improved your balance, flexibility, and strength.
Your physiotherapist will help you decide which assistive aides will be required following surgery and when those aides can safely be discontinued.
Outcomes
How Your New Knee Is Different
Improvement of knee motion is a goal of total knee replacement, but restoration of full motion is uncommon. The motion of your knee replacement after surgery can be predicted by the range of motion you have in your knee before surgery. Most patients can expect to be able to almost fully straighten the replaced knee and to bend the knee sufficiently to climb stairs and get in and out of a car. Kneeling is sometimes uncomfortable, but it is not harmful.
Most people feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending activities.
Most people also feel or hear some clicking of the metal and plastic with knee bending or walking. This is a normal. These differences often diminish with time and most patients find them to be tolerable when compared with the pain and limited function they experienced prior to surgery.
Your new knee may activate metal detectors required for security in airports and some buildings. Tell the security agent about your hip replacement if the alarm is activated. You may ask your orthopaedic surgeon for a card confirming that you have an artificial knee.
Protecting Your Knee Replacement
There are many things you can do to protect your knee replacement and extend the life of your knee implant
- Participate in a regular light exercise program to maintain proper strength and mobility of your new knee
- Take special precautions to avoid falls and injuries. If you break a bone in your leg, you may require more surgery
- Make sure your dentist knows that you have a knee replacement. You should be given antibiotics before all dental surgery for the rest of your life
- See your orthopaedic surgeon periodically for a routine follow-up examination and x-rays, usually once a year, even if your knee replacement seems to be doing fine.
Extending the Life of Your Knee Implant
Currently, more than 90% of modern total Knee replacements are still functioning well 15 years after the surgery. Following your orthopaedic surgeon’s instructions after surgery and taking care to protect your knee replacement and your general health are important ways you can contribute to the final success of your surgery.